Collaborative Innovation: How Biotech Partnerships Are Driving Solutions for Joint Diseases
Exploring Business Strategies to Meet the Demand for Joint Disease Therapies

Joint diseases such as osteoarthritis (OA) and rheumatoid arthritis (RA) are becoming increasingly prevalent due to aging populations and lifestyle factors. The global joint disease therapy market is projected to grow significantly in the next decade, creating opportunities for biotech companies to develop innovative solutions.
Biotech-Research Partnerships: A Model for Success
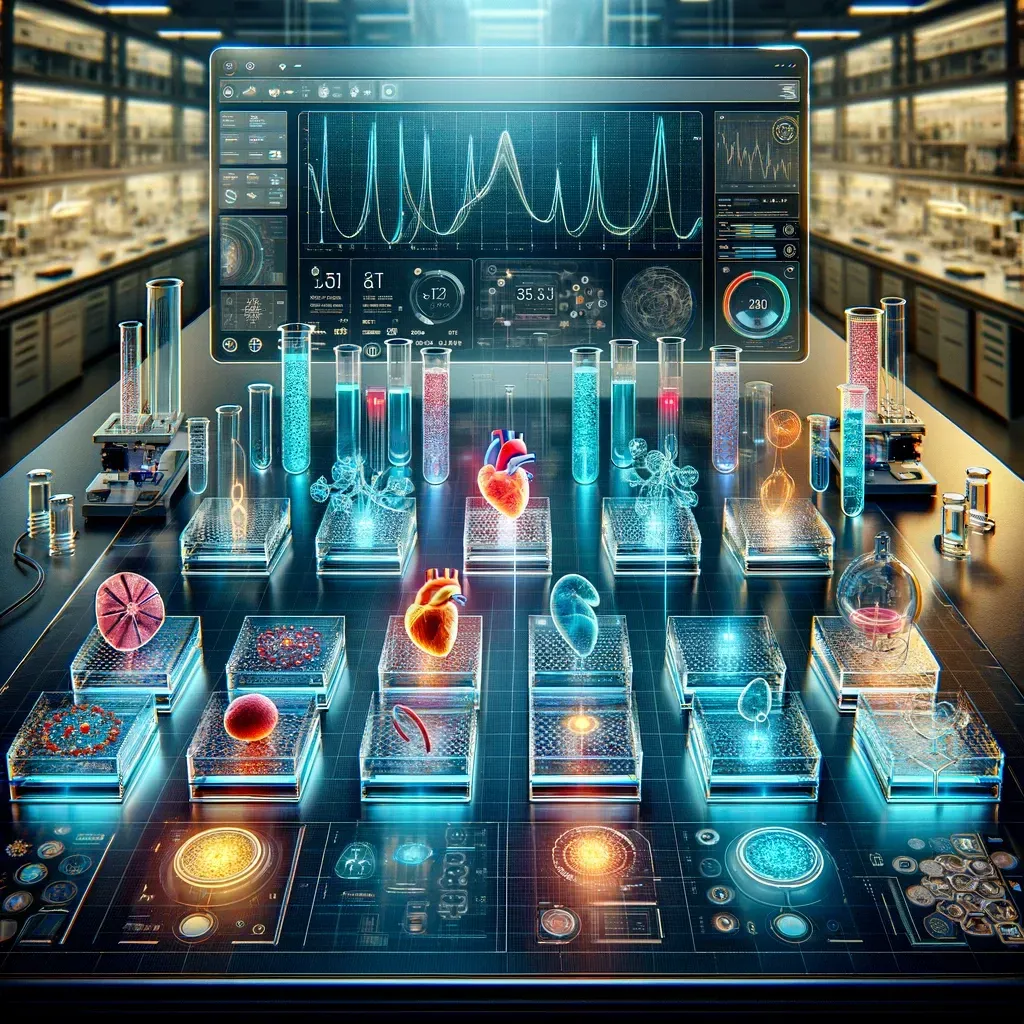
Collaborative efforts between biotech firms and academic research institutions are playing a pivotal role in advancing joint disease therapies. These partnerships combine cutting-edge technology from industry leaders with groundbreaking discoveries from academic labs, expediting the journey from concept to clinical application. A notable example includes the use of organ-on-a-chip platforms co-developed by biotech companies and universities.
Investment Opportunities in Joint Disease Research
As the demand for joint disease therapies grows, the sector is attracting increased attention from investors. Venture capital and private equity firms are recognizing the potential for high returns in funding biotech startups focused on joint health. These investments are not only fueling R&D but also enabling firms to scale up their operations.
Overcoming Commercialization Challenges
Bridging the gap between research and commercial viability remains a significant challenge. However, strategic partnerships are helping biotech companies navigate regulatory pathways, optimize production costs, and effectively market new therapies. By leveraging shared resources and expertise, these collaborations are reducing time-to-market and increasing accessibility for patients.
Biotech News